I would have NEVER posted a picture of a raccoon with a rabies article, simply due to the fact that 99% of all confirmed rabies cases in Erath County originate from the skunk. The other 1% goes to the bats.
So here is the full article with statistics!
Know your Neighborhood Wildlife - The Real Facts about Rabies
by TOM PIPERSON & BIRGIT SOMMER
Have you ever wondered about the dangers of rabies? Birgit Sommer, licensed wildlife rehabilitator and director of the Rainbow Wildlife Rescue in Stephenville, deals with these issues on a regular basis and would like to set the record straight about some urban legends surrounding the rabies virus.
Even though we enjoy the benefits of 21st Century medicine, rabies is still dangerous and even deadly to its victims, both animal and human. Understanding the facts about rabies, as provided in this article, can help prevent the spread of the disease, or even save a life.
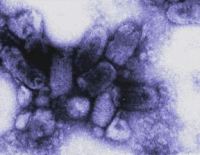
1. What exactly is rabies?
Answer:
Rabies is a contagious virus that can cause death in people and certain animals and is nearly always fatal if not treated in a timely manner.
2. How is rabies transmitted?
Answer:
The rabies virus is usually transmitted through the saliva of an infected animal, most commonly through a bite. The virus can be transmitted from animal to animal, from animal to human, and on rare occasions, from human to human.
Another way of transmitting the virus, even though highly uncommon, is for saliva or brain tissue from a rabid animal to get directly into the eyes, nose, mouth or open wound of a person or animal.
However, contrary to common belief, you can’t get rabies from the blood, urine, or feces of an infected animal.
During her survey, Ms. Sommer noted another misconception about rabies transmission. She stated it is not true that an animal can be just a carrier of the rabies virus and transmit it to another animal or humans for weeks, months or even years.
According to the CDC, "No person in the United States has ever contracted rabies from a dog, cat or ferret held in quarantine for 10 days."
Before the rabies virus reaches the brain, the animal does not show any symptoms, according to the CDC. The animal does not appear ill during this time, called the incubation period, which may last for weeks or months. During this time period the animal CAN NOT transmit the virus to another animal or person. This is the reason why animals that have bitten a human are held in quarantine for 10 days.
As the CDC states, " Only late in the disease, after the virus has reached the brain and multiplied there to cause an encephalitis (inflammation of the brain) does the virus move from the brain to the salivary glands and saliva."
3. What animals are most likely to have rabies?
Answer:
All mammals can get rabies. It is most common in un-vaccinated household pets such as dogs, cats and ferrets as well as in livestock such as cattle, and wild animals like skunks, bats, raccoons, coyotes and foxes.
Small animals like mice, rats, squirrels, and even opossums, are almost never found to be infected with rabies. According to the Centers for Disease Control and Prevention, bites by these animals are usually not considered a risk of rabies unless the animal was sick or behaving abnormally and rabies is a major problem in your vicinity.
4. How common is rabies in Erath County?
Answer:
Officially confirmed rabies cases from 2000 until today include according to the Texas Department of State Health Services Infectious Disease Control Unit:
| Year | Rabies Cases | Confirmed In | Variant |
| 2000 | 24 | 23 skunks, 1 cat | Skunk |
| 2001 | 27 | 27 skunks | Skunk |
| 2002 | 8 | 6 skunks, 1 goat, 1 horse | Skunk |
| 2003 | 10 | 8 skunks, 2 dogs | Skunk |
| 2004 | 4 | 2 skunks, 1 bat, 1 cattle | Skunk, Bat |
| 2005 | 5 | 3 skunks, 1 cat, 1 cattle | Skunk |
| 2006 | 2 | 1 skunk, 1 dog | Skunk |
| 2007 | 4 | 3 skunks, 1 cat | Skunk |
| 2008 | 6 | 3 skunks, 2 dogs, 1 raccoon | Skunk |
| 2009 | 2 | 1 skunk, 1 cat | Skunk |
All animals except 1 (the bat in 2004) contracted the virus from an infected skunk.
5. How can I tell if an animal has rabies?
Answer:
The symptoms are not easily recognized because other diseases display similar symptoms. Pets infected with the rabies virus act in unusual ways. Be alert for changes in behavior. A dog that is friendly may avoid people. Mean dogs may act friendly to strangers. Animals may become aggressive, make strange noises or erratic movements, and attack other animals or humans. They may have trouble walking, drinking, swallowing, or chewing. It may not be able to close its mouth, and may appear to be choking. If you see an animal acting like this, call the local animal control agency right away.
6. What should I do if I had contact with a possibly rabid animal?
Answer:
Prompt treatment is required to prevent a rabies infection. First, flush the bite or wound area with water for at least one full minute. Follow up by washing with soap (or detergent if soap is not immediately available) to remove saliva containing the virus. Then apply a disinfectant such as rubbing alcohol, bleach, or iodine tincture directly on the wound and under skin flaps to stop the rabies from being absorbed into the body tissue. Then get to your doctor or an emergency room as soon as possible.
7. How is rabies diagnosed in animals and humans?
Answer:
A direct fluorescent antibody test (dFA) is used to test the brain tissue of animals suspected to be rabid. However, the dFA test can only be performed after the animal has died. For humans, several tests are required to diagnose rabies. Samples of body tissues and fluids - saliva, spinal fluid, serum, and hair follicles - are tested for signs of the rabies virus. Positive results from one test is not proof of rabies, all tests are required for diagnosis.
8. Can baby animals have rabies?
Answer:
Babies born to a healthy rabies-free mother will be rabies free at birth. Babies born to a rabid mother will most likely have rabies, because it is exposed to the mother’s saliva. These babies will probably not survive long enough to go out into the world. Teach your children to never touch wildlife. Call the authorities or your local wildlife rehabilitator if you find a wild baby animal that seems to be orphaned and in need of human intervention.
9. How do I protect myself and my pets from rabies?
Answer:
- Have a veterinarian vaccinate your dogs and cats against rabies. By law, you need to do this every year, or every three years, depending on the type of vaccine used.
- Keeping your pets vaccinated protects you and them.
- Keep pets away from wildlife and don’t let them wander loose through the neighborhood.
- Avoid contact with wild animals and with dogs and cats you do not know. Do not try to hand-feed wild animals and do not keep them as pets.
- Do not touch sick or injured animals. Call and report them to the authorities.
10. How do I prevent the spread of rabies?
Answer:
Be a responsible pet owner and have all your pets vaccinated once a year.
- Keep your pets confined and supervised.
- Spay or neuter your pets to prevent the spread of unwanted and unvaccinated animals straying through your neighborhood.
- Enjoy wild animals such as raccoons, skunks, and foxes from afar. Do not handle, feed, or attract wild animals with open garbage cans or litter. Do not leave pet food outside!
- Do not rescue wild animals or bring them into your home. Do not try to raise orphaned wildlife. Call animal control or your local wildlife rehabilitator for assistance.