Know your Neighborhood Wildlife - The Real Facts about Rabies
by TOM PIPERSON & BIRGIT SOMMER
June 17, 2009
Getting the facts about rabies is not easy. Myths and misconceptions are as strong today as they were 4,000 years ago when rabies was first recognized. When the average person today thinks about rabies, they typically imagine dogs gone wild, foaming at the mouth, and painful shots. Ignorance about rabies can be hazardous to your personal health and well being, as well as the safety of family members, beloved pets and livestock. Understanding the facts about rabies, as provided in this article, can help prevent the spread of the disease, or even save a life.
Fact – You cannot contract rabies from an animal held in quarantine for 10 days.
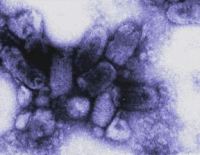
If an animal who seems ill or acts strange happens to bite you, it is possible you could be infected with the rabies virus. The virus is typically spread through the saliva of an infected carrier in the late stages of the disease after it has reached the brain. From thousands of years of medical observation of rabies victims, it is known that 3-5 days after reaching the brain, the animal will show unmistakable symptoms of rabies. A few extra days of quarantine are added as a precaution.
Fact – Until the rabies virus reaches the brain, a bite from an infected animal does not transmit the disease to its victim.
The period between the time a victim is bitten by a rabid animal and the time it can spread the infection to others is called the incubation period. It can take a few weeks up to several months for the virus to transfer from muscle tissue, to a peripheral nerve, the central nervous system, the brain, and from there into the saliva. This incubation time can depend on age (shorter in children), the location of the bite (the farther away from the head, the better), and the severity of the bite.
Fact – A person cannot contract rabies from the blood, feces or urine of an infected animal, or from handling a carcass that is dried or mummified.
Only saliva or nerve tissue (brain, spinal cord) from a rabid animal can transmit the virus to another victim.
It is possible to contract rabies through an open wound or mucous membrane. One possible scenario would be by contact with a water dish contaminated with saliva from a rabid dog. Or by breathing the air in a cave where rabies-infected bats are present. Human transplants who died of rabies infection have proven that nerve tissue transmits the virus, as well.
Fact – Bats can bite a victim without leaving a visible trace and present a unique danger for rabies infection.
Bats also carry the rabies virus. People who are awake will feel a pinch when bitten by a bat. But, when asleep, the bat’s needle-like teeth make practically no wound and may not even be felt. Because a few cases have proven rabies as the cause of death in individuals found asleep in a room with a bat, state governments have taken special steps to educate their residents.
In Iowa, for example, the public health department presents a detailed decision tree for the public to use in diagnosing suspected cases of bat-infected rabies, and recommends administering the rabies post-exposure prophylaxis (PEP) in cases where a person who has fallen asleep in the same room as a bat cannot say with certainty “I know I wasn’t bitten.”
In Colorado, based on the epidemiology of rabies, the primary rabies exposure risk for domestic pets is from bats. The Colorado Public Health Department recommends prompt treatment of pets for any direct exposure to bats, such as if direct physical contact was observed, the presence of puncture wounds on the bat or pet, or the presence of saliva or injuries on the bat.
Fact – Rabies is rare in opossums, rodents, and squirrels.
Small rodents (mice, rats, guinea pigs, hamsters, chipmunks, squirrels) are almost never found to be infected with rabies and have not been known to cause rabies among humans in the United States. According to the Centers for Disease Control and Prevention, bites by these animals are usually not considered a risk of rabies unless the animal was sick or behaving abnormally and rabies is a major problem in your vicinity.
Opossums have naturally evolved their metabolism to resist many common infections, as well as having a robust immune system virtually impervious to the venom of rattlesnakes, vipers such as cottonmouth snakes, and spiders. Their extremely low body temperature of 94 to 97 degrees F is an inhospitable environment for survival of the rabies virus and other common wildlife diseases. There have been only 5 confirmed cases of a rabies infected opossum in Texas since 1962.
Fact – Human-to-human transmission of rabies is possible, but very rare.
There have been 8 confirmed cases of death due to human-to-human rabies transmission as the result of a corneal transplant operation.
Fact – The signs of rabies in an infected animal are not easily recognized.
Foaming at the mouth can be a symptom of many conditions more common than rabies, such as roundworms, ticks, poisoning, liver failure, allergies, distemper, and dehydration. It is important to remember it is the total package of symptoms that add up to a possible diagnosis of rabies. Be alert for changes in behavior.
A dog that is normally friendly may avoid people. Dogs that are not normally sociable may act friendly to strangers. Animals may become aggressive, make strange noises or erratic movements, and attack other animals or humans. They may have trouble drinking, swallowing, or chewing. A direct fluorescent antibody test (dFA) is used to test the brain tissue of animals suspected to be rabid. However, the dFA test can only be performed after the animal has died.
Fact – Thoroughly cleaning and treating the bite or wound area significantly reduces the chance of infection.
Immediate treatment is required in order to prevent possible rabies infection. First, flush the area with water for at least one full minute. Follow up by washing with soap (or detergent if soap is not immediately available) to remove saliva containing the virus. Then apply a disinfectant such as alcohol, bleach, iodine tincture directly on the wound and under skin flaps to stop the rabies from being absorbed into the body tissue. Get to your doctor or an emergency room as soon as possible.
Fact – The symptoms of rabies in humans are numerous and increases in severity as the disease progresses.
Some of the symptoms identified in rabies victims include twitching or tingling around the area of the animal bite, fever, sore throat, difficulty in speaking, confusion, aggressiveness, nausea, abdominal pain, muscle aches and spasms, paralysis, seizures, hydrophobia (fear of drinking or swallowing water, painful spasms when trying to drink), diplopia (double vision), breathing difficulties.
Fact – Treatment for rabies in humans who have been bitten by a rabid animal is 100% effective if given within 24 to 48 hours after the bite occurred.
Post-exposure rabies anti-serum costs about $1,200. Patients in the US receive one dose of human rabies immunoglobulin, or HRIG, and five doses of rabies vaccine administered over a 28 day period, at day 0, day 3, day 7, day 14 and day 28. One half the dose of the HRIG is injected in the region of the bite, if possible, with the remainder injected into muscle tissue away from the bite. Previously, the immunoglobulin was injected through the abdominal wall with a large needle which was extremely painful.
Fact – Vaccination of animals and humans can greatly reduce the spread of rabies.
Vaccination of wild animal reservoirs through food baited with rabies vaccine has controlled the spread the disease in Europe. At one point the virus was almost completely eradicated in the regions treated before rabies started to reappear from wild and imported animals. Wild animals such as the red fox account for 4 times the number of rabies cases as domestic animals in France.
Domestic animal vaccination programs are the law in many municipalities across America. Typically, a dog or cat that is not current with rabies vaccinations and has a wound of unknown origin must be quarantined at a veterinary hospital at the owner’s expense or at home under the supervision of the department of agriculture or public health. Some pet owners cannot afford the cost of quarantining and are required, by law, to euthanize their pet. States such as Pennsylvania have set up vaccination clinics costing $10 to encourage residents to obey the law requiring all domestic dogs and cats three months of age or older to be inoculated against rabies.
Fact – New treatments and vaccines hold promise for eventually and permanently ending rabies everywhere.
In over 4000 years, when the rabies virus was first recognized, slow but steady progress was made in the fight against rabies. It wasn’t until the late 19th Century when the original rabies vaccine, harvested from infected rabbits, was formulated by Louis Pasteur and Emile Roux, back in 1885. The modern vaccine, formulated in the late 1960s, uses purified and cultured cells grown and harvested in sterile labs. Biological research and advances in technology continue to bring the world closer to eliminating rabies completely and forever.
Today, the vast majority of human deaths caused by rabies occur in Asia and India. The industrialized world, including countries such as New Zealand and Australia, much of Western Europe, and the United States, have much lower rates of death from rabies.
Human vaccination is essential for animal care professionals, lab technicians and anyone who may come in contact with the rabies virus in the course of their work or hobby. The vaccination consists of a series of shots given in the arm or shoulder and must be renewed on a regular basis. Since the potential for exposure is high among certain individuals, vaccines are effective in preventing rabies infections. Overseas travel to locations known for high incidence of infection is another circumstance where administration of the human rabies vaccination series is highly recommended.
Summary
Provide your pets and livestock with rabies vaccine as advised by your family veterinarian. Keep rabies pet vaccines current.
Keep pets away from wildlife and don’t let them wander loose through the neighborhood.
Contact the proper authorities if you see an animal acting strangely. Never attempt to catch or touch the animal unless you are trained.
If your pet is bitten by an animal, call the animal authorities and take your pet to the vet.
If a person is bitten by an animal (whether it is from a wild skunk caught foraging in the trash or a nip on the hand from a neighbor’s pet), clean the wound thoroughly and go to your doctor or medical clinic for treatment. Contact the authorities who will try to capture the animal for testing or quarantine.
Keep contact information handy for notifying the proper authorities about a possible rabid animal in the neighborhood.
Information and research provided by Birgit Sommer, licensed wildlife rehabilitator in the State of Texas and Director of the Rainbow Wildlife Rescue.